In January of 2020, the Centers for Medicare and Medicaid Services (CMS) proposed a new rule that could increase the out-of-pocket costs for people who take prescription medication for hepatitis B in the U.S. The proposed rule states that health insurance companies would be able to collect patient coinsurance through pharmaceutical manufacturer financial assistance. However, the insurance companies will be allowed to disregard any coinsurance paid with copay assistance when calculating how much the patient has paid toward their deductible and annual out-of-pocket (OOP) limit.
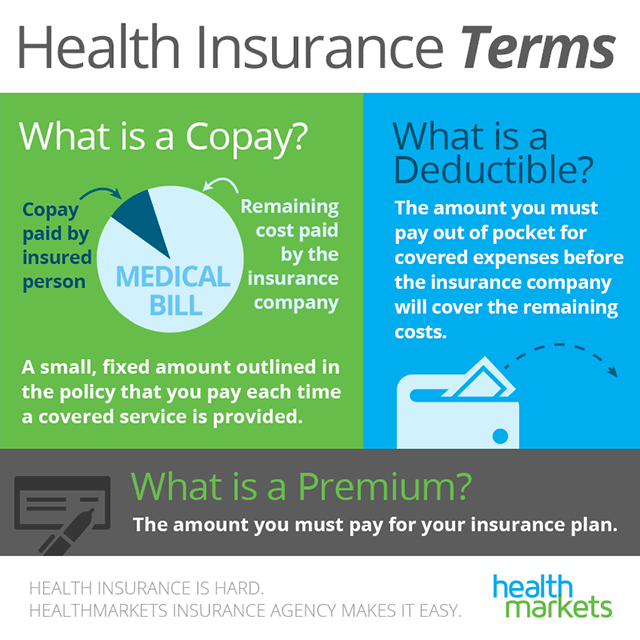
If you’re fortunate enough to have employer-provided insurance, the company typically picks up part of the premium. Copay: A predetermined rate you pay for health care services at the time of care. Definition; Level 1 – Generic: Copay. Generic drugs are as effective, safe and high quality as their brand-name counterparts, yet less expensive. Learn more about generic drugs. Level 2 – Brand-name: Copay or coinsurance. Considered “preferred” when there is no generic, and because of their value and effectiveness.
This proposal – titled 2021 Notice of Benefit and Payment Parameters – reverses a recent ruling that would have required health insurance companies to count the value of manufacturer copay assistance toward an enrollee’s annual deductible and OOP limit in most circumstances1. This rule acknowledged that manufacturer copay assistance helps lessen the financial burden of medications for patients. In the US, prescription drugs can be extremely costly, making manufacturer’s copay assistance programs necessary for many patients. For example, brand name treatments are often expensive in order to help pharmaceutical companies earn back the costs of the research and time spent making the medication. Sometimes, the brand name treatments are the only ones that are available, like Vemlidy, or the only version that a person can take. A reversal of the rule would mean that hepatitis B patients and those living with other chronic illnesses may have to pay a larger amount of out-of-pocket costs for their medications.
Overnight respite care (in-home or onsite care designed to give family caregivers a break, available up to 30 days each calendar year) Overnight geriatric evaluations (evaluations by a team of health care providers to help you and your family decide on a care plan) Copay amount for. SPOTLIGHT & RELEASES The Qualified Medicare Beneficiary (QMB) program provides Medicare coverage of Part A and Part B premiums and cost sharing to low-income Medicare beneficiaries. In 2017, 7.7 million people (more than one out of eight people with Medicare) were in the QMB program. A copay is a fixed amount you pay for a health care service, usually when you receive the service. The amount can vary by the type of service. How it works: Your plan determines what your copay is for different types of services, and when you have one. You may have a copay before you’ve finished paying toward your deductible.
To understand the significance of this change, we first need to understand what a copay accumulator is.
What is a Copay Accumulator Program and How Does It Work?
A copay accumulator – or accumulator adjustment program – is a strategy used by insurance companies and Pharmacy BenefitsManagers (PBMs) that stop manufacturer copay assistance coupons from counting towards two things: 1) the deductible and 2) the maximum out-of-pocket spending. What does this mean?
Previously, a person could receive financial assistance from companies that make a drug, and that would count towards their deductible and/or out-of-pocket costs, depending upon the insurance plan. Pharmaceutical companies often provide financial assistance (such as a co-pay card) to help underinsured individuals afford expensive medications. This means that the person paying for the drug would end up saving money, often thousands of dollars.
Ms office 2019 in windows 7. Why Is This an Issue?
As the AIDS Institute explains it, “ … the trend in health insurance benefit design is to shift more of the cost of health care to patients through high deductibles and coinsurance rates …In order to afford the medicine they need, patients increasingly rely on manufacturer copay assistance.” With copay accumulators, the individuals who need assistance the most will be unable to receive it, and will end up paying more for their treatments.
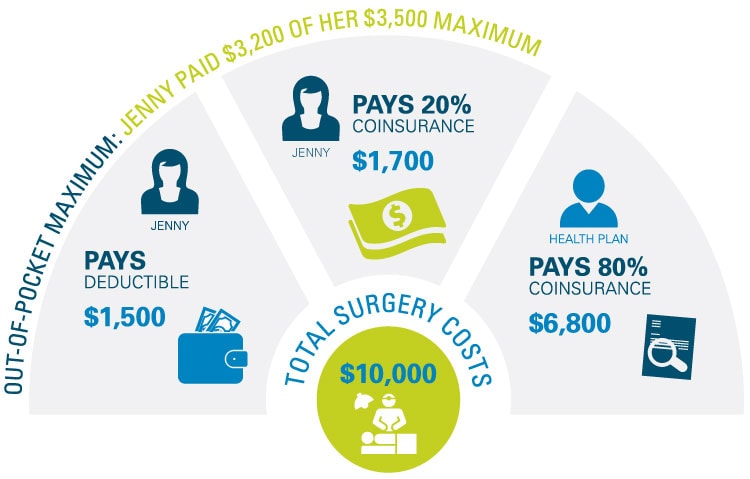
Below is an example of a copay accumulator program from the Patient Access Network (PAN) Foundation:
As shown in the above image, with a copay accumulator program – meaning her manufacturer’s assistance is no longer counted toward her out-of-pocket limit- the consumer ends up paying more, while the insurance company is able to reduce the amount they are paying.
Copay accumulator programs are making life-saving treatments increasingly inaccessible. Research shows that the more out-of-pocket costs a person has to pay, the more likely they are to abandon their medication. Once on a hepatitis B medication, stopping suddenly or only taking it once in a while can cause flares and lead to an even higher risk of liver damage.
In the United States, many of those who are living with hepatitis B come from underserved populations with limited access to healthcare. Oftentimes, cultural differences and language barriers can make it difficult to access and utilize the services they need. Now, copay accumulators are making the navigation process even more complex and placing a higher cost burden on patients.
1The rule required insurance companies to count manufacturer copay assistance toward a patient’s deductible and OOP limit for all brand name drugs for which there is no generic alternative and in cases where the patient gained access to the brand name drug through an insurance plan’s appeals or exceptions process.
Pcp Copay Meaning
A new type of policy has been introduced that has the potential to put cancer patients at serious financial risk. You may not have heard of copay accumulators or accumulator adjustment programs before, so this blog will provide an overview of these policies to help prepare you in case you might be at risk of facing this barrier to affordable cancer care.
First Things First…
Before we talk about this new type of policy, it might be helpful to define some terms.
The term accumulator refers to the running total of a patient’s costs that apply towards their deductible and out-of-pocket maximum
A deductible is the amount a patient pays for health care services before insurance kicks in. For example, a patient with a $2,000 deductible would pay for their first $2,000 of care before health insurance begins to cover costs.
Hack for bloons monkey city. A copayment is a fixed amount a patient pays for a covered health services after they’ve paid their deductible. For example, you might pay a $20 copayment when you visit your doctor.
An out-of-pocket maximum is the most amount of money a patient has to pay for covered services in a plan year. After this amount is spent on deductibles, copayments, and coinsurance, a health plans pays 100% of the cost of covered benefits.
A high deductible health plan is a plan with a higher deductible than a traditional insurance plan. The monthly premium is usually lower, but patients pay more health care costs out of their own pocket before the insurance company starts to pay.
A pharmacy benefit manager (PBM) is a third-party administrator of prescription drug programs contracted by health plans, employers, unions, and government entities to manage prescription drug programs.
A copayment card can be provided by a pharmaceutical company (aka a manufacturer) or a charity. These cards help patients afford the cost of their prescriptions. The amount of the patient’s copayment may be reduced or covered completely if they use a copayment card.
What are co-pay accumulators or accumulator adjustment programs?

Co-pay accumulators or accumulator adjustment programs are relatively new policies that some pharmacy benefit managers and insurers are using to prohibit manufacturer copayment cards or other forms of manufacturer assistance from being used to pay down a patient’s deductible or out-of-pocket maximum.
What does this mean for patients?

It means that when your copayment card limit has been reached, the value on the card will not have counted toward your deductible or annual out-of-pocket maximum. Instead, you will need to pay your full deductible before cost-sharing protections kick in. In other words, when a patient uses a copayment card, the amount of money that the card is “worth” does not count towards the patient’s deductible or out-of-pocket maximum. Therefore, the patient is responsible for significantly more money to cover the cost of their health care and prescriptions.
Let’s walk through an example…
$0 Copay Meaning
It’s the start of a new health plan year in January and you are on a medication with a price of $3,000 a month. You use your manufacturer copay card at the pharmacy and make a regular copayment at the counter. For example, that copayment might cost you $20 each month instead of $3,000 each month. By the time March arrives, you’ve reached the limit on your copay assistance. As a result, when you go to refill your prescription in April, you will owe the full $3,000 cost of the drug, because the deductible has not yet been paid down.
Insurance Copay Meaning
Will you be ready for an unexpected out of pocket cost?
We are concerned that patients may not know they are enrolled in these programs and may not be prepared to pay the full cost of their deductible right away. While you might have received a disclosure from your insurer, it may not have been completely clear what the practical implications of this new policy would mean.
Who is enrolled in these programs?
People most likely to be enrolled in these programs are those in employer-sponsored plans and those in high-deductible health plans (HDHPs) in particular. HDHPs are becoming increasingly common as plans employers and insurers use to help incentivize appropriate health care utilization and to lower costs.
If you have been affected, or think you might be in one of these programs and want to be prepared, what can you do?
- Consult your health plan materials or call your insurer to ask questions. If you have been affected by this type of policy and have had to switch to another drug or have been unable to fill your prescription, tell your insurer.
- Tell your employer, too. If you are employed and receive health insurance through your job, tell your employer. They may have adopted this program thinking of it as a cost-savings strategy without truly understanding the negative impact it could have on their employees.
- Tell us! We want to know about your experience so we can be better informed when we are advocating for you. Contact us at action@cancersupportcommunity.org.
Copay Meaning Healthcare
This blog was written in collaboration with The Arthritis Foundation.
